
Log on to Availity ® to request a claim review and initiate a negotiation (independent dispute resolution-IDR) for NSA-eligible services. This section provides a quick introduction to filing claims with BCBSIL. If you do not have a contract with us, claims for certain services may be eligible for payment review under the No Surprises Act (NSA). Other audits will be conducted as needed, such as diagnosis-related groups (DRG) validation, site of care, readmission, etc.
Participating providers can contact your local Network Management office if you have any questions concerning the process for claim reviews. Blue Cross conducts audits in accordance with Medicare laws, rules and regulations. Mail the completed Claim Review form, along with any attachments, to the appropriate address indicated on the form. Primary carrier's EOB indicating claim was filed with the primary carrier within the timely filing deadline.Documentation from BCBSTX requesting additional information.Documentation from BCBSTX indicating claim was incomplete.Above documentation indicating that the claim was filed with the wrong division of Blue Cross and Blue Shield of Texas.Availity Electronic Batch (EBR) Response Reports.Services denied for failure to meet timely filing requirements are not subject to reimbursement unless the provider presents documentation proving a corrected claim was filed within the applicable. Certified Mail Receipt (only if accompanied by TDI mail log) Corrected claims filed beyond federal, state-mandated, or company standard timely filing limits will be denied as outside the timely filing limit.Overseas claims Please refer to the claims filing information on page 106 of this brochure. Note: Once we pay benefits, there is a five-year limitation on the re-issuance of uncashed checks. The claim review process for a specific claim will be considered complete following your receipt of the 2nd claim review determination.įor those claims which are being reviewed for timely filing, BCBSTX will accept the following documentation as acceptable proof of timely filing: Note: Timely filing for overseas pharmacy claims is limited to one year from the prescription fill date.If your clam has been overturned after reviewing, your payment/PCS will serve as your notification.If your claim has been maintained after review, you will receive a written notification of the claim review determination.BCBSTX will complete the second claim review within 45 days following the receipt of your request for a second claim review. For long or continuing inpatient stays, or other long-term care, you should submit claims at least every 30 days.
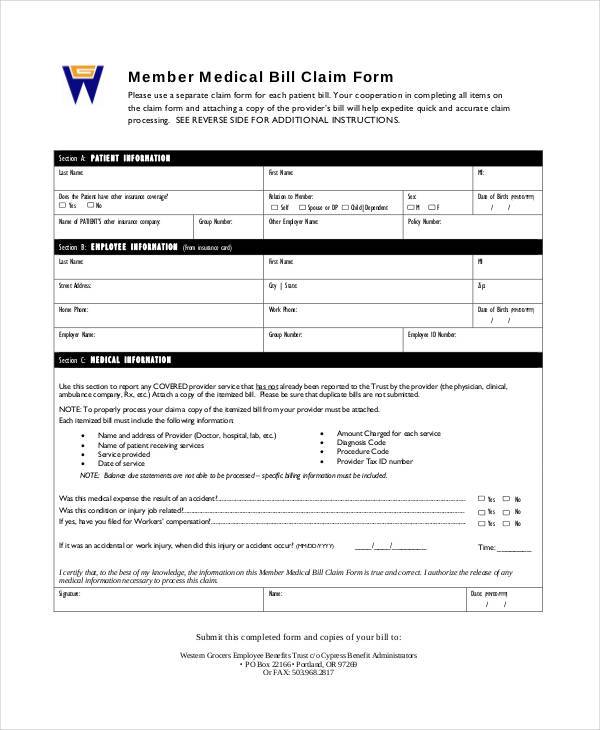
If the claim review determination is not satisfactory to you, you may request a second claim review. Use a separate claim form for each family member.


 0 kommentar(er)
0 kommentar(er)
